Over 750k people are diagnosed with myocardial infarction in the United States every year, and a new JAMA paper suggests that far more of those patients are incorrectly diagnosed than many might expect.
Because of the clinical and medicolegal consequences of incorrectly discharging an MI patient, medical practices and clinical research have largely focused on addressing MI underdiagnosis. However, evidence continues to mount that MI overdiagnosis could actually be more common:
- A review of patients with clinically diagnosed MI found that 9% of those events would have been reclassified as myocardial injury after expert review.
- Another review of clinical trials with central adjudication committees identified 15% to 20% fewer MIs than site investigators originally reported.
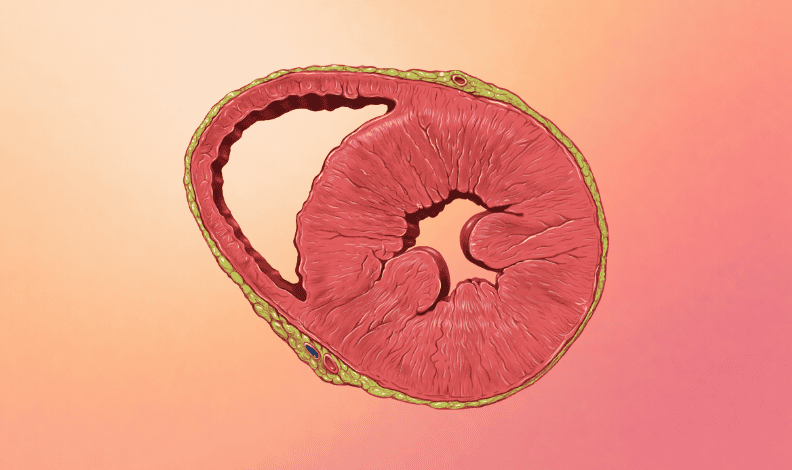
- A CMRI study revealed that only half of patients with clinically diagnosed MI had an infarction pattern on their cardiac MRI exams, leading to alternative diagnoses (e.g. myocarditis) for one-fifth of the participants.
So what’s causing this trend towards MI overdiagnosis? The authors believe that the current MI diagnosis criteria (symptoms of coronary ischemia + abnormal troponin levels) isn’t sufficient, and the liberal use of troponin testing (particularly in the US) has compounded this problem.
- One study revealed that a quarter of all ED visitors underwent a troponin test, even though less than half of them had chest pain.
- Another study showed that roughly one in seven ED patients had elevated troponin, even though they weren’t experiencing an MI, in part because troponin can be a sign of other non-coronary diseases.
- Current troponin thresholds are based on cohorts of young or middle-aged adults, and many patients who receive troponin tests are older.
In other words, we’re giving more low-probability patients highly sensitive troponin tests, and there’s “a complete lack of understanding” about troponin-based MI diagnosis, leading to a surge in false-positive MI cases.
In order to reduce MI overdiagnosis, the authors suggest…
- Enacting laws limiting malpractice payments (and limiting defensive medicine)
- Limiting troponin testing to higher-probability patients
- Considering new age-specific troponin thresholds
- Adopting new AI-based MI detection solutions
- Developing new biomarkers for MI detection
- Using cardiac imaging for ambiguous cases
- Better adherence to the MI guidelines
The Takeaway
MI overdiagnosis might not get the headlines, but there’s a strong chance that it’s now more common than MI underdiagnosis, leading to a cascade of unnecessary testing, treatments, costs, and stress. We need more research to confirm this theory, and we’d need some big changes if it proves to be true.