|
Echo AI Improves LVEF | HF + AS Outcomes
April 6, 2023
|
|
|

|
|
Together with
|
|
|
|
“The best humans are still better than AI… However, AI does allow for more consistency and precision.”
|
|
Cedars-Sinai David Ouyang, MD after showing that echo AI can indeed improve LVEF exams.
|
|
|
|
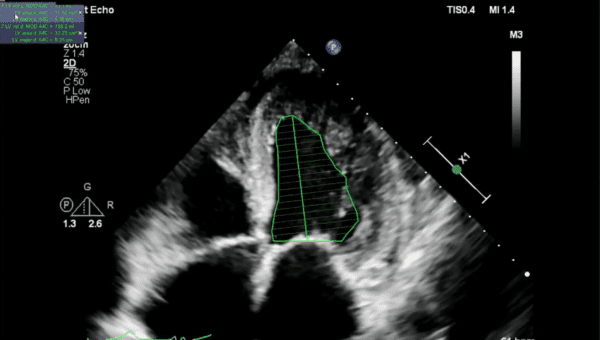
Cedars-Sinai researchers published what might be the strongest evidence yet of AI’s ability to improve echocardiography workflows and accuracy.
The researchers randomized 3,495 transthoracic echo LVEF studies to be assessed by either a Cedars-Sinai-developed AI tool or expert sonographers (within the standard cardiology PACS workflow), before final assessments by blinded cardiologists.
This was the first blinded RCT evaluating an echo AI solution, and one of the first for any imaging AI solutions.
Echo AI nailed the study’s primary endpoint, as the final cardiologist assessments required substantial LVEF changes (>5% change) far less often with AI-based studies than those from the sonographer group (16.8% vs. 27.2%).
The echo AI solution AI further supported its advantage over sonographer assessments, producing…
- A smaller average LVEF difference between the initial and final cardiologist assessments (2.79% vs. 3.77%)
- A smaller average LVEF difference between the final cardiologist assessments and patients’ previous/historical cardiologist assessments (6.29% vs. 7.23%)
- Faster average initial LVEF assessments (AI 131 seconds faster)
- Faster median cardiologist LVEF assessments (54 vs. 64 seconds)
The blinded cardiologists also often couldn’t tell whether AI or the human sonographers produced the initial assessments (43%), while predicting the correct assessment source only slightly more often than the incorrect source (32% & 24%).
The Takeaway
This study shows that AI-based LVEF assessments can be “non-inferior and even superior” to initial assessment by sonographers, while also reducing labor and variability throughout the echo workflow.
Even though previous echo AI research has produced similar results and this study only used data from a single center, the fact that it was echo AI’s first blinded RCT is very notable, and bolsters the growing body of evidence supporting AI’s ability to improve echo workflows in the real world.
|




|
|
Start Measuring What Matters
Looking to optimize your cardiovascular imaging services, but don’t know what to measure? Check out this Change Healthcare report for insights on how to track and evaluate your cardiovascular imaging performance, assess quality, and enhance operational efficiency. Read the full article now and start measuring what matters!
|
|
A New Standard of Heart Care
Open to a more personalized and proactive approach to cardiovascular care? Check out this video detailing Cleerly’s unique approach to heart disease risk assessments and care.
|
|
Democratizing Echocardiography with AI
We talk a lot about AI’s potential to expand echo access, and this Imaging Wire Show reveals that ultrasound’s AI-driven expansion might go far beyond what many of us had in mind. Check out our discussion with Duke Health’s Madhav Swaminathan, MBBS, MD and Us2.ai’s Carolyn Lam MBBS, PhD and James Hare, to see how AI is democratizing echo exams.
|
|
- Smartwatch-Grade ECGs Predict CV Events: UCL researchers used data from 54k UK Biobank participants to show that 15-second single lead ECG (smartwatch-grade) could predict increased risk of heart failure (median age 58, avg. follow-up 11.5 years). After adjusting for confounding factors, an extra beat coming from the lower chambers of the heart was linked to a twofold increase in heart failure (HR: 2.09). A separate sample of 29k participants verified those results, while also finding that an extra beat from the top chambers nearly doubled the likelihood of Afib (HR: 1.8).
- HF + Aortic Stenosis Outcomes: A JACC study involving 9,133 HFrEF patients showed that those with moderate and severe AS had a much higher chance of either dying or being hospitalized for heart failure over three years than patients without AS (62% vs. 46%). Interestingly, HFrEF patients with severe AS had fewer hospitalizations than moderate AS patients (36.2% vs. 43.6%), possibly because they were more likely to undergo aortic valve replacement surgery.
- FDA Med Device and AI Changes: The FDA published a draft guidance on how it will regulate updates to AI/ML algorithms in response to new data. The guidance is designed to promote innovation by allowing AI/ML medical devices to more easily learn from local conditions (e.g. diagnostic devices could be built to adapt to the data of individual facilities). In other regulatory news, Section 3305 of the Omnibus is in effect as of last week, meaning that companies can’t market medical devices without first showing the FDA a solid cybersecurity plan.
- Empagliflozin Boosts Health Status: It’s probably no surprise that patients with HFpEF have impaired health status, but the SGLT2 inhibitor empagliflozin (Jardiance) can allow significant improvements. A team of researchers assessed the KCCQ scores of nearly 3k participants with HFpEF, discovering that factors such as older age, being female, and having high BMI, anemia, and a history of diabetes and CKD were all tied to worse health status scores. empagliflozin improved health status across all of these vulnerable subgroups in just 12 weeks, with obese patients experiencing the most benefits.
- Getinge’s Pump Problems: Getinge’s Cardiosave intra-aortic balloon pumps are having a tough few weeks after EU regulators forced it to suspend pump sales and the FDA issued a Class I recall for several pumps. The FDA’s recall stems from complaints that Getinge Cardiosave pumps have shut down without warning, a problem that Getinge plans to address through a software update. Meanwhile Getinge’s European suspensions were due concerns about risk management, post-market surveillance, and its ability to promptly correct field safety problems.
- Spotting High-Risk MI Patients with OCT: A JACC study highlighted optical coherence tomography’s ability to help identify high-risk heart lesions and predict which MI patients are likely to experience another cardiac event. Analysis of OCT exams from 883 patients with acute MI revealed that OCT-identified thin-cap fibroatheroma (TCFA) and minimal lumen area (MLA) <3.5 mm2 independently predicted adverse events over a median of 3.3 years (adjusted hazard ratios: 3.05 & 3.71).
- Cholesterol’s Deadly J-Curve: A Nature Scientific Reports study discovered that critically ill patients with low levels of certain types of cholesterol (LDL-C, HDL-C, and TC) face higher death risks. Analyzing data from 27k critically ill patients, researchers found a “J-shaped” connection between cholesterol types and all-cause and noncardiovascular mortality, with the greatest risks when cholesterol levels dropped below 96 mg/dL (LDL-C), 27 mg/dL (HDL-C), and 140 mg/dL (TC). The findings suggest that low LDL-C and low HDL-C combine to amplify mortality risks.
- Preventative Coverage Overruled: A Texas federal judge struck down an Affordable Care Act mandate requiring health plans to fully cover preventative services, including some key cardiology-related screenings (diabetes, heart disease) and treatments (statins). The ruling stated that the task force that recommended the coverage was unconstitutional because its members were neither appointed by the president nor confirmed by the Senate. The ruling takes effect immediately, but the HHS has already appealed the decision, potentially giving the Supreme Court another chance to direct the future of the ACA.
- Ventura’s COVID Cardiac Arrests: Cedars-Sinai researchers found that Ventura County, California’s rates of out-of-hospital sudden cardiac arrests (OHCA) surged during the COVID pandemic. Ventura County recorded 1,315 OHCAs during the four years pre-pandemic and 907 OHCAs during the first two years of the COVID pandemic, representing a significant increase overall (39 to 54 per 100k citizens annually) and an even greater increase among the county’s Hispanic population (38 to 68 per 100k citizens). Outcomes were also worse, as OHSCA survival fell from 15% to 10%.
- Omics-Based Hypertension Diagnosis: A European research consortium will use €15M in funding to develop omics-based personalized hypertension diagnostic tools. The new HT-Advance project expands upon previous efforts to develop multiomics biomarkers to distinguish patients with endocrine and primary hypertension, and will now use AI to analyze various biomarkers that could help define patients’ underlying hypertension causes and more accurately select treatments.
- EPs on CMS Ablation Cuts: The Heart Rhythm Society’s latest survey (585 U.S. electrophysiologists) regarding CMS’ catheter ablation reimbursement cuts revealed widespread EP concerns that could drive big practice changes. The vast majority of EPs felt their practices were either “somewhat” or “significantly” affected by the cuts (89% & 67%), so it’s no surprise that many anticipated making changes to their patient panels and payer mix to stabilize practice revenues (78%). As a result, the majority of respondents expect that CMS’ cuts will reduce patient access (85%).
|
|
The HeartFlow Story
Shifting the standard of care is a monumental undertaking, and yet physicians across the globe are embracing HeartFlow’s FFRct Analysis. Hear from the co-founder how HeartFlow got its start, and why physicians love it.
|
|
Reducing ECG Background Noise
Monebo’s Kinitec Rhythms ECG Algorithm separates true ECG signals from background noise, leading to more accurate diagnoses and improved operator efficiency. See for yourself how the algorithm measured up to a gold standard.
|
|
PIA’s Post-Processing Solution
Advanced cardiac imaging often calls for a time-consuming post-processing step, requiring costly software, hardware, and training. See how PIA provides this post-processing at lower cost, improved consistency, and greater efficiency.
|
|
|
|
|