|
Exercise is Medicine | Cardiac Nuclear-CT Guidelines
September 15, 2022
|
|
|

|
|
Together with
|

|
|
|
“The best way to a man’s heart is through the fourth and fifth rib.”
|
|
An embroidered message tweeted by Ali Neitzel, MD
|
|
|
|
The JACC published a four-part series last week in which experts spotlight exercise as a means of cardiovascular disease reduction, prevention, and treatment. The second paper in the series received a lot of attention, with one cardiologist speculating that it may be the best paper of the year.
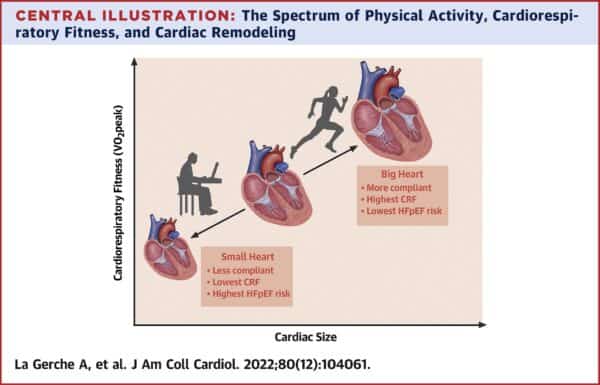
The paper in question argues that a subgroup of patients with heart failure with preserved ejection fraction (HFpEF) have rarely exercised throughout their life. As a result, they have smaller hearts that do not adequately protect from heart failure during the aging process.
It’s well established that consistent exercise results in increased cardiac mass, stroke volume, cardiac output, and peak oxygen consumption. But does physical inactivity lead to cardiac atrophy, reduced output, and reduced heart chamber size? The authors say yes.
The paper cites nearly one hundred studies in support of its claim. Here are the highlights:
- There is a strong association between physical activity, cardiorespiratory fitness, and heart function.
- Aging results in a smaller, stiffer heart, but regular exercise mitigates these effects.
- Physical inactivity leads to reduced output, smaller heart chamber size, and less ability to improve cardiac performance in the future with exercise.
- A chronic lack of exercise is a major risk factor for HFpEF.
The Clinical Implications
Thinking of HFpEF as an exercise deficiency syndrome will help physicians better understand the condition, recognize risk earlier, and most importantly, provide a clear path to prevention. The authors recommend consistent exercise, especially before the age of 60, after which exercise intervention benefits are usually modest.
The Takeaway
The fact that exercise is good for heart health may not be earth-shattering, but this literature review underscores the role of exercise as a major HFpEF risk factor. The authors propose that a subset of HFpEF patients have hearts that are smaller because they’ve been underexercised, making regular physical activity an effective prevention strategy.
|




|
|
A New Cardiac Population Health Pathway
Nanox.ai’s cardiac solution analyzes already-existing non-gated CT scans and quantifies each patient’s CAC, giving clinicians a valuable tool for detecting cardiovascular disease and predicting future cardiovascular events.
|
|
A New Standard of Heart Care
Open to a more personalized and proactive approach to cardiovascular care? Check out this video detailing Cleerly’s unique approach to heart disease risk assessments and care.
|
|
- Photon-Counting CT Plaque Characterization: A new study out of Switzerland highlighted photon-counting CT technology’s (PCD-CT, an emerging CT tech) advantage over standard CT for coronary plaque characterization. Researchers analyzed exams from 20 coronary syndrome patients undergoing ECG-gated coronary CT angiography (w/ PCD-CT), finding that PCD-CT reduced blooming artifacts, which improved visualization of fibrotic and lipid-rich plaque components in ultra-high contrast mode.
- FDA Approves Edwards’s TEER Solution: Edwards Lifesciences announced that its PASCAL Precision mitral valve transcatheter edge-to-edge repair (TEER) system received FDA approval for the treatment of degenerative mitral regurgitation (DMR). The PASCAL Precision system is designed for predictable capture, positioning, and release, and is already CE-marked for patients with both mitral and tricuspid regurgitation. The solution joins a handful of other transcatheter repair therapies in Edwards’ portfolio.
- Cardiac Nuclear-CT Guidelines: The ASNC and three other major nuclear imaging and cardiac CT societies released a new set of guidelines for using hybrid nuclear-CT cardiac imaging. The 45-page guideline goes step-by-step on how to prepare a lab for SPECT/CT and cardiac PET/CT imaging, including new recommended training requirements, models for cross-specialty study interpretation, and suggested solutions for reimbursement challenges.
- LVEF in BAV Disease: New findings suggest that left ventricular ejection fraction (LVEF) values that are used to signal the need for surgical intervention may be too restrictive among people with bicuspid aortic valve (BAV) disease. Current guidelines recommend surgery when LVEF drops below 50%, but data from 2.7k patients with BAV indicate that risk increases significantly when LVEF is below 60%. In a multivariable analysis, people with LVEF in the 50-59% range were 83% more likely to die from any cause.
- BAC Risk Demographics: A team of New York-based researchers provided new insights into how demographics impact patients’ risk of having breast arterial calcifications (BAC) in their screening mammograms, noting that BAC is a possible biomarker for coronary artery disease. A review of 17k women’s mammograms (12.3% w/ BAC) found that BAC risks were far greater among racial minorities (e.g. Hispanic women have 2.7-fold greater risk vs. non-Hispanics) and older women (e.g. women aged 55-64yrs have 6-fold greater risk of BAC vs. women <44yrs).
- Simple Tool to Predict ATTR-CM: Mayo Clinic researchers devised a simple clinical score to identify HFpEF patients at increased risk of transthyretin amyloid cardiomyopathy (ATTR-CM). Researchers used data from 666 patients to develop a point-based risk score that was based on six variables: age, male sex, hypertension diagnosis, EF less than 60%, posterior wall thickness of 12 mm or more, and relative wall thickness more than 0.57 (score range −1 to 10). In an external cohort (n=66), the model showed strong discriminatory performance (AUC: 0.84).
- RPM Use Extremely Concentrated: A Health Affairs study sparked a ton of conversation last week after finding that just 0.1% of “high-volume providers” accounted for 69% of all general remote patient monitoring use (n = 20M MA enrollees, Jan. 2019 – March 2021). The authors also found that only 0.75% of all physicians had any RPM claims, causing them to conclude that there’s still plenty of runway for RPM growth as more physicians adopt new tech.
- DASH Diet Could Prevent CV Events: UCSF researchers suggest the DASH diet is better at preventing heart attack and stroke among people with hypertension compared to other lifestyle adjustments. In a simulation study using the latest US statistics for stage 1 hypertension, the authors found that adherence to the Dietary Approaches to stop Hypertension (DASH) diet coupled with other behavior modifications could prevent up to 26k CVD events and 2.9k deaths while saving $1.6B in associated healthcare costs over the course of a decade.
- FDA Expands Boston Scientific’s WATCHMAN Approval: The FDA has approved an expanded indication for Boston Scientific’s WATCHMAN FLX left atrial appendage close device to include a 45-day dual antiplatelet therapy option for patients immediately following the implantation. The 45-day option serves as an alternative to the 45-day anticoagulation plus aspirin regimen. The WATCHMAN FLX is used to prevent stroke in patients with nonvalvular AFib, and the expanded labeling has been available in Europe since 2017.
- Cardiac POCUS Fast Learners: An Indiana University study found that after a brief training session (video + 10min hands-on lesson), medical students with little cardiac POCUS experience were able to obtain high-quality PSLA images and diagnose cardiac tamponade. Among 132 second-year medical students who completed the training, 72% obtained PSLA cardiac views without instructor guidance and 62% were able to identify pericardial effusion and diagnose cardiac tamponade (all with simulated patients).
- HBR Data Measurement Improvements: An HBR article penned by several noteworthy thought leaders highlighted the need for better metrics to track the ever-increasing amount of health data – particularly quality measures that don’t rely on medical claim lines. The authors outlined four imperatives for establishing that system: 1) reduce the cost of data collection by adopting wearables; 2) incorporate this data with information from EHRs, PROMs, and SDOH; 3) enhance EHRs to help clinicians personalize care using these data sources; and 4) standardize clinical measures for final quality measurements.
|
|
Us2.ai’s Echo Evidence
Have more echo studies than sonographers? See how Us2.ai was able to classify, segment, and annotate echocardiographic videos with similar accuracy as expert sonographers.
|
|
User Experience and Cardiovascular Imaging Transformation
Check out this Change Healthcare video discussing the importance of user experience in the adoption of structured reporting, and how it can lead to improvements in imaging speed, quality, and cardiologist workflow.
|
|
|
|
|