|
Groundbreaking AFib Study | Predicting Heart Attack Outcomes
June 27, 2022
|
|
|

|
|
Together with
|

|
|
|
“You can’t improve what you don’t measure.”
|
|
Editor-in-Chief of Journal of Cardiac Failure, Robert Mentz, MD, on including self-reported gender identity, race, and ethnicity when evaluating journal submissions.
|
|
|
Surgeries & Interventions
|
|
|
|
|
|
The debate around atrial fibrillation ablation procedures gained clarity last week, when the groundbreaking DECAAF II trial revealed that more aggressive treatment did not lead to better patient outcomes – and even increased health risks for patients with advanced AFib.
The DECAAF II trial, spearheaded by Tulane University researchers, studied 843 AFib patients (44 medical centers, 10 countries) between July 2016 and January 2020, with follow-up through February 2021.
Half of the patients received the standard care, pulmonary vein isolation treatment (PVI), while the other half received MRI-guided atrial fibrosis ablation in addition to the standard PVI. The more aggressive MRI-guided treatment allowed doctors to use a digital 3D map of the patient’s heart to ablate diseased tissue more thoroughly and precisely. Follow-up analysis revealed:
- There was no significant difference in atrial arrhythmia recurrence between the PVI + fibrosis-guided ablation group and PVI alone group (43% vs. 46%; P = 0.63).
- Patients in the fibrosis-guided + PVI group were more likely to experience an adverse event, such as stroke, PV stenosis, bleeding, heart failure, or death (2.2% vs. 0%).
- 1.5% of patients in the fibrosis-guided + PVI group had an ischemic stroke compared to none in the PVI-only group.
- Two deaths occurred in the fibrosis-guided ablation + PVI group (one which may have been procedure-related).
The Takeaway
This team of Tulane researchers pushed the field of atrial fibrillation forward last week, finding that MRI-guided atrial fibrosis ablation for treating persistent AF is not superior to conventional catheter ablation. The revelation surprised many cardiologists, underscoring the importance of large, prospective, randomized clinical trials.
|




|
|
- Predicting Adverse Cardiac Remodeling: Research presented at SNMMI’s annual conference found that the new PET radiotracer 68GA-FAPI-46 helped predict functional outcomes after a heart attack. The researchers used the radiotracer in PET/CT scans to detect cells with activated fibroblasts in 35 patients within 11 days of acute myocardial infarction. When they paired the PET findings with information from cardiac MRI, they found that the extent of FAP upregulation – even in the tissue surrounding the acute infarction site – predicted subsequent adverse outcomes. The image that captures these findings also won SNMMI Image of the Year.
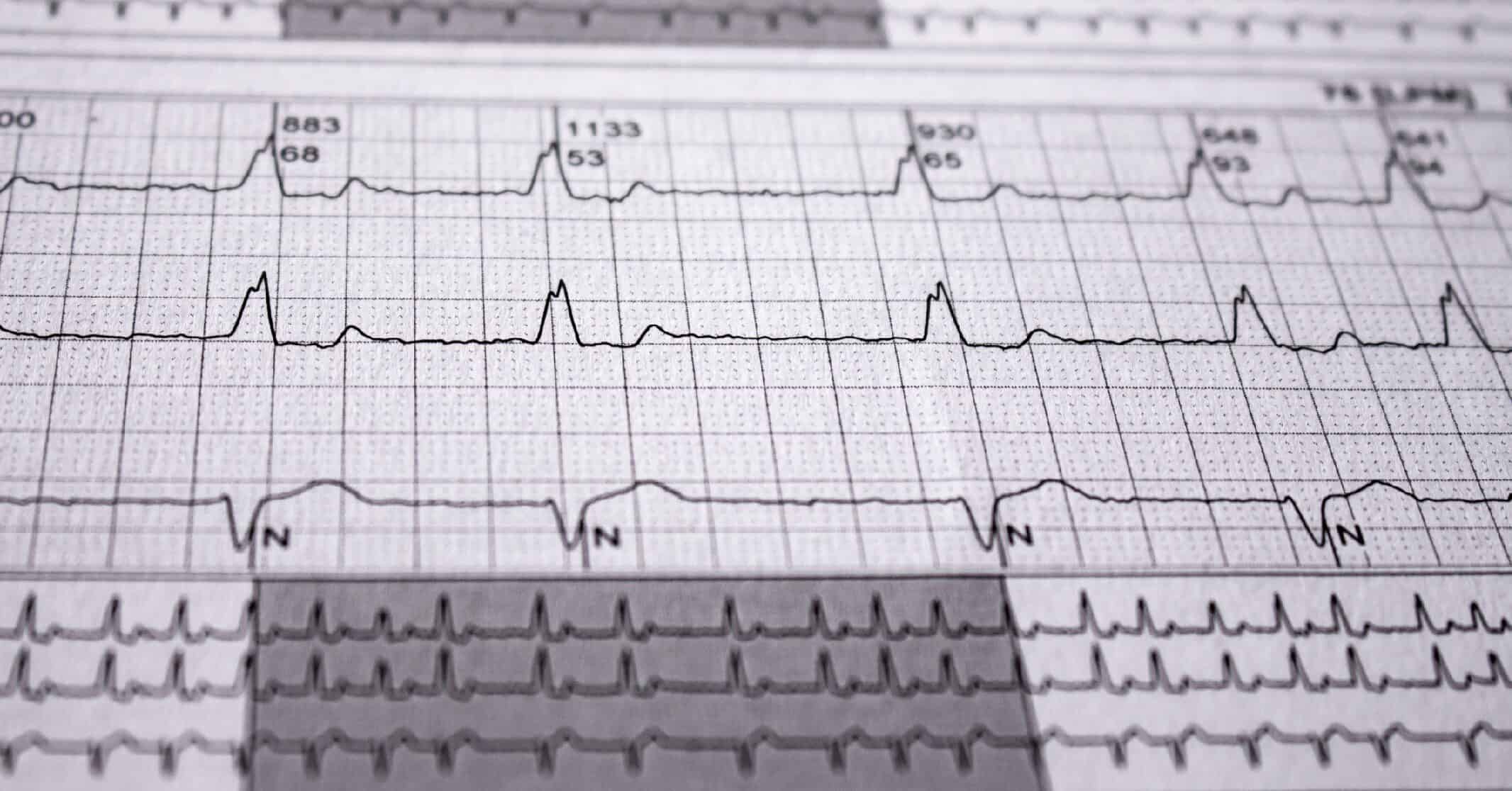
- Idoven Series A: Idoven secured €18.5M in Series A funding to support the development of its ECG analysis software, Willem. The AI-based platform can identify over 80 cardiac patterns and produce a list of probable arrhythmias, risk scores, and alerts.
- 7 Tips for Cath Labs: Amid the ongoing contrast shortage, Cleveland’s University Hospitals health system shared seven tips that helped them decrease cath lab contrast use by nearly 46%. Here they are: (1) replace automated injection systems with manifold, except for TAVR procedures; (2) restrict catheterization procedures to interventionalists; (3) minimize contrast angiography by considering more definitive tests early on; (4) limit optical coherence tomography; (5) closely monitor contrast use; (6) consider using CO2 angiography and IVUS for peripheral cases; and (7) redistribute contrast to smaller vials to reduce waste.
- Statins & Arterial Stiffness: A new study out of China finds that statins may slow the progression of arterial stiffness. Researchers assessed 5,105 high-risk adults’ brachial-ankle pulse wave velocity (baPWV) and found that statin users were associated with lower baPWV at baseline (difference: -33.6 cm/s). When the measurement was repeated ~4.8 years later, statin users had significantly slower progression of baPWV compared to non-statin users (difference: -23.3 cm/s per year; 410 statin users & 410 non-statin users). People who stopped taking statins, or didn’t take it consistently, didn’t experience these benefits.
- inHEART’s FDA Clearance: inHEART Medical received FDA clearance for its new inHEART MODELS software suite. The solution uses CT and MRI images to build an interactive 3D model of a patient’s heart that physicians can reference before and during ventricular tachycardia ablation procedures. With this clearance, inHEART will focus on expanding its commercial footprint in the U.S.
- The Monotherapy Advantage: Among patients with AFib and stable CAD, those who received rivaroxaban alone had a 38% lower risk of cardiovascular and bleeding events than those who received combination anticoagulant and antiplatelet therapy. After comparing thrombotic, bleeding, and fatal event rates, a team of Japan-based researchers found the monotherapy group (n=1,107) boasted a lower mortality rate (3.7% vs. 6.6%) and had a lower risk of subsequent events (hazard ratio, 0.62) compared to the combination group (n=1,108).
- DiA & Intelerad Partner: DiA Imaging Analysis announced a partnership with Intelerad Medical Systems, combining its LVivo Seamless AI-based cardiac ultrasound analysis system with Intelerad’s IntelePACS solution. The alliance bolsters Intelerad’s cardiac ultrasound capabilities while further expanding DiA’s list of PACS and ultrasound partners (ScImage, Change Healthcare, GE, Philips, Konica, Terason, Sonoscape, Circle CVI, Watson Health).
- 69,000 Stents Recalled: Atrium Medical recalled 68,800 iCast Covered Stents after receiving 75 complaints (9 injuries, no deaths). The FDA classified this as a Class I recall– the most severe kind. Customers reported issues with balloon or catheter hub separation during delivery system removal from the patient, potentially causing significant harm. Atrium Medical issued a letter to its customers detailing instructions on how best to deflate the balloon and withdraw the delivery system safely.
- Beta-Blockers for PCI: A study out of China revealed that early beta-blocker therapy decreased major in-hospital bleeds in patients undergoing percutaneous coronary intervention for acute coronary syndrome. Researchers gave 36% of 43,640 patients oral beta-blockers within 24 hours of therapy. They found that early administration reduced in-hospital bleeding risk by 52% and mortality risk by 53%. Both high- (≥50mg/day) and low- (<50mg/day) dose users saw bleeding risk reduction (39% and 53%, respectively) compared to non-users.
- Tackling Cardiac Xenotransplantation: Brigham and Women’s Hospital report five looming barriers researchers must address to bring “humanized” porcine heart xenotransplantation to the clinical realm. Here’s a rundown of the obstacles: (1) Immune reactions from the recipient, (2) infectious porcine viruses, (3) physiological barriers like xenograft overgrowth, (4) social and ethical hurdles associated with community and animal rights group acceptance, and (5) Implementation differences in private versus public healthcare spheres.
- Elucid’s Series B Funding: Elucid locked in $27M in Series B funding to support the development of its FDA-cleared and CE-marked software, Elucid Vivo. The solution uses CT angiography and AI to identify and quantify heart attack-causing tissue in the arterial wall, potentially helping physicians diagnose the direct cause of chest pain and determine if patients have early-stage heart disease. The new investment brings the company’s total funding to nearly $50M.
- ACH-Test Safety: A JACC meta-analysis confirmed the safety of intracoronary acetylcholine testing procedures. The authors pooled data from 16 studies (12,585 patients) and found major complications in 0.5% of patients, none of which were fatal. When researchers analyzed the data by subgroups, they did find that major complications were more likely to occur in Asian versus Western populations (2.3% vs. 0%) and when the studies followed contemporary diagnosis criteria for epicardial spasm defined as ≥90% diameter reduction versus 75% reduction (1% vs. 0%).
|
|
|
|
|