|
Chest CT’s Untapped Potential | Statins vs. Aspirin
June 6, 2022
|
|
|

|
|
Together with
|

|
|
|
“Routine reporting of CAC on all chest CT examinations…could identify a large number of patients with previously unknown CAC who might benefit from preventive treatment.”
|
|
Toronto General Hospital researchers.
|
|
|
|
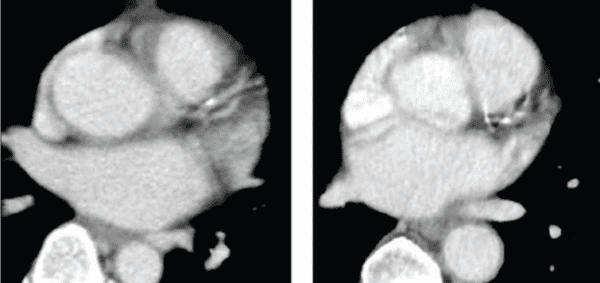
A new AJR study out of Toronto General Hospital highlighted the largely-untapped potential of non-gated chest CT CAC scoring, and the significant impact it could have with widespread adoption.
Current guidelines recommend visual CAC evaluations with all non-gated non-contrast chest CTs. However, these guidelines aren’t consistently followed and they exclude contrast-enhanced chest CTs.
The researchers challenged these practices, performing visual CAC assessments on 260 patients’ non-gated chest CT exams (116 contrast-enhanced, 144 non-contrast) and comparing them to the same patients’ cardiac CT CAC scores (performed within 12-months) and ~6-year cardiac event outcomes.
As you might expect, visual contrast-enhanced and non-contrast chest CT CAC scoring:
- Detected CAC with high sensitivity (83% & 90%) and specificity (both 100%)
- Accurately predicted major cardiac events (Hazard ratios: 4.5 & 3.4)
- Had relatively benign false negatives (0 of 26 had cardiac events)
- Achieved high inter-observer agreement (κ=0.89 & 0.95)
The Takeaway
Considering that CAC scores were only noted in 37% of the patients’ original non-contrast chest CT reports and 23% of their contrast-enhanced chest CT reports, this study adds solid evidence in favor of more widespread CAC score reporting in non-gated CT exams.That might also prove to be good news for the folks working on opportunistic CAC AI solutions, noting that AI has (so far) seen the greatest adoption when it supports processes that most radiologists are actually doing.
|




|
|
- Statins Over Aspirin: A new RSNA study confirmed that statins are far more effective than aspirin for maintaining cardiovascular health. The researchers identified 2,815 participants with nonobstructive CAD and 3,125 without detectable plaque. Over a ~5.7yr follow-up period, the nonobstructive CAD participants who were taking statins at baseline had lower rates of major cardiac events (9.5% vs. 13%), mortality (8.25% vs. 10.8%), and myocardial infarction (4.28% vs. 5.1%) than those not taking statins. Meanwhile, participants taking aspirin had worse outcomes than those not following any therapy (MACE: 14.7% vs. 10.9%; mortality 10.85% vs. 9.59%; MI: 6.2% vs. 4.38%). Neither therapy showed benefits among participants without plaque.
- Hello Heart Funding: Cardiac digital therapeutics company Hello Heart closed a $70M Series D funding round to support “significant growth in customer demand” after doubling its number of employer clients in the last three months alone. The press release left the total client count a mystery, but did reveal that the solution is now available to “millions of members.” Hello Heart’s program includes a wireless blood pressure cuff and a mobile app that helps track metrics such as pulse, medications, and weight, then delivers personalized recommendations to reduce the risk of cardiovascular disease.
- CT-FFR’s Pre-TAVR Impact: A new JACC study added more evidence for using CT-FFR before TAVR procedures, showing that it’s more accurate than CCTA and could reduce unnecessary invasive coronary angiographies (ICA). Analysis of 76 patients with significant coronary stenosis (≥1) who underwent pre-TAVR CCTA exams showed that CT-FFR outperformed CCTA for sensitivity (84.6% vs. 76.9%), specificity (88.3% vs. 64.5%), and diagnostic accuracy (87.6% vs. 66.9%). These results suggest that a CT-FFR–guided approach could avoid ICA in 57.1% of patients, versus 43.6% with CCTA.
- Miga Health Funding: App developer Miga Health closed a $12M seed round to create a heart health consumer brand similar to Headspace or Duolingo and combine it with clinical care. The funding will be used to develop an app that will allow patients to monitor their blood pressure from home before connecting them to educational content and clinical services to address their needs.
- The Fallacy of Zero CAC: A new JACC editorial highlighted the “false sense of cardiac health” created by zero calcium scores. The author cited a growing field of research showing that many patients with zero CAC scores have detectable plaque on CCTA, and that follow-up CCTAs commonly show non-calcified plaque progression. Given the new solutions supporting automated coronary plaque quantification and the growing evidence of what CAC scanning misses, the author urged adopting CCTA-based approaches for symptomatic patients.
- Detecting Weak Heart Pumps: This week brought more good news for cardiac patients after Mayo Clinic announced that it successfully developed an AI algorithm that can interpret single-lead EKG tracings from an Apple Watch to identify patients with a weak heart pump (left ventricular dysfunction). The algorithm was trained on 125k Apple Watch EKGs from over 2,400 participants, resulting in a final AUC of 0.88 that makes it as good or slightly better than a medical treadmill test. If verified, the algorithm could enable consumer grade wearables to help diagnose weak heart pumps outside of the medical setting, allowing for earlier treatment of the potentially fatal condition.
- Patients’ AI Perspectives: A new JAMA study suggests that most patients (n = 926 in 2019) are optimistic about the impact of healthcare AI, although a lot of that depends on how AI is used. The majority of respondents believed that AI would make health care either “much” or “somewhat” better (10.9% & 44.5%), while 19% “did not know” how AI would impact care, and just 4.3% believed AI would make health care “somewhat” worse. Perhaps more notable, most patients were “very” or “somewhat” comfortable with AI reading a CXR (12.3% & 42.7%), but far fewer felt that way about AI making cancer diagnoses (6% & 25.2%).
- Chest Pain Disparities: Women wait 11 minutes longer than men to be evaluated for chest pain in the ER (48 min vs. 37 min) and are less likely to be admitted to the hospital following evaluation (12% vs. 18%), according to an American Heart Association analysis of 29M ER visits between 2014 and 2018. The study also found that Black patients waited 10-15 minutes longer to receive care for chest pain in the ER compared to white patients, leading the authors to call for more research to uncover if the differences are related to variation in hospital care quality or location.
- Heart Failure RPM: A UPenn study found no difference in 12-month readmissions and mortality rates between heart failure patients with usual post-discharge care (n = 280) or those in a remote monitoring program that included a digital scale, a smart bottle for diuretics, and financial incentives for providing daily measurements (n = 272). The results add to the growing body of research indicating that financial incentives do little to change behavior when not paired with other patient engagement protocols like coaching or automated reminders.
- Diagnosing Physician Error: An interesting study published in The Quarterly Journal of Economics used a machine learning model to predict patients’ probability of a heart attack, then identified cases where physicians’ testing decisions deviated from predicted risk. The approach revealed two major inefficiencies: 1) physicians overtest (predictably low-risk patients are tested but do not benefit), 2) physicians undertest (predictably high-risk patients are left untested then go on to suffer adverse health events). The researchers make the case that the simultaneous over- and undertesting is likely due to systematic errors in judgment, such as overweighting factors like chest pain, and suggest that care models should place a larger emphasis on physician error to mitigate these risks.
|
|
|
|
|